Elevance Health Boston Consulting Group Matrix
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
Elevance Health Bundle
What is included in the product
Tailored analysis for Elevance's portfolio across the BCG Matrix.
Export-ready design for quick drag-and-drop into PowerPoint to save time during presentations.
Preview = Final Product
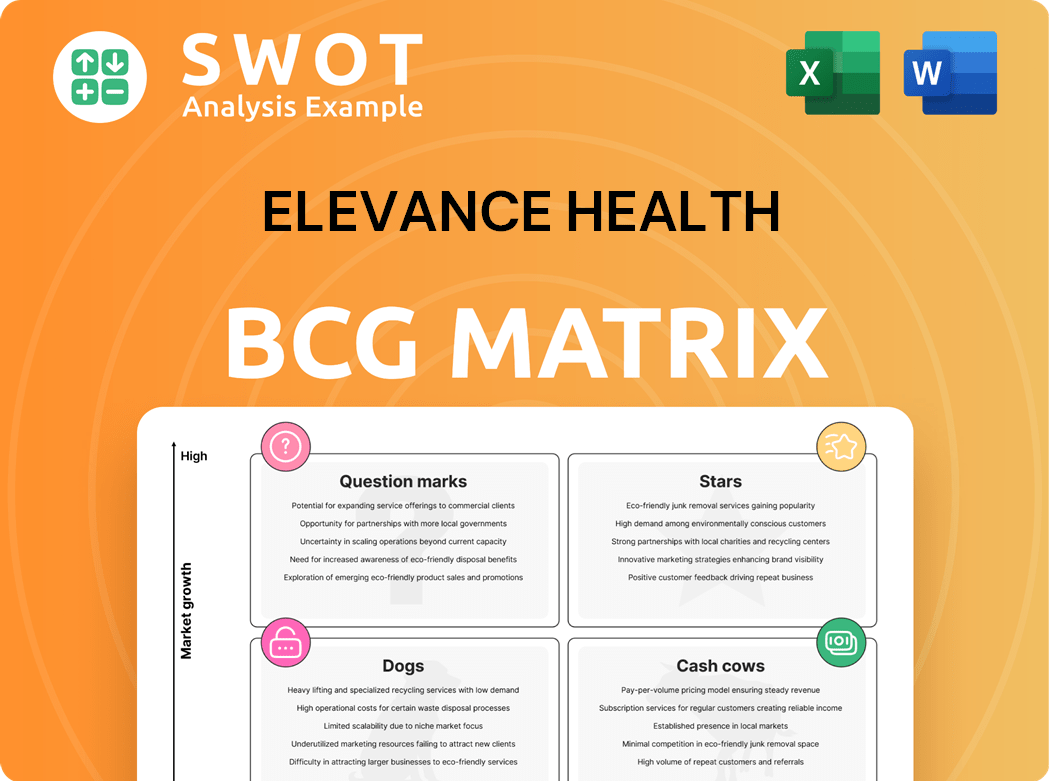
Elevance Health BCG Matrix
The BCG Matrix preview mirrors the final document post-purchase. This is the complete, professionally formatted report on Elevance Health, ready for immediate use.
BCG Matrix Template
Elevance Health's BCG Matrix offers a glimpse into its diverse portfolio. Discover the potential of its products across four key quadrants: Stars, Cash Cows, Dogs, and Question Marks. Understand where Elevance Health excels and where it faces challenges in a dynamic market. This preview only scratches the surface of the strategic landscape. Get the full BCG Matrix report to uncover detailed quadrant placements, data-backed recommendations, and a roadmap to smart investment and product decisions.
Stars
Elevance Health anticipates a 7% to 9% increase in Medicare Advantage (MA) membership in 2025. This growth reflects a robust market presence, supported by consistent benefit offerings and enhanced member retention rates. The company's strategic focus on local market dynamics further solidifies its leadership in the MA sector. In 2024, UnitedHealth Group's Medicare Advantage enrollment grew, reaching approximately 8.6 million members.
Carelon Services, part of Elevance Health, is seeing substantial growth, exceeding its long-term revenue targets. In 2024, Carelon's revenue growth is projected to be above the long-term target range, fueled by internal and external expansion. This growth supports Elevance Health's focus on whole health risk. Carelon's contribution is critical to the company's success.
Elevance Health's ACA exchange plans are shining stars. The individual exchange business saw over 30% growth in 2024, a testament to their appeal. This success is fueled by innovative and affordable products. They are well-positioned in a competitive market.
Commercial Fee-Based Membership
Elevance Health's commercial fee-based membership is flourishing, reflecting a solid value proposition to employers. This segment's growth signals its leadership in the commercial market. In 2024, the company's revenue from this area has increased substantially. This expansion is a clear indicator of its competitive edge.
- Revenue growth in the commercial fee-based segment.
- Strong value proposition for employers.
- Leadership position in the commercial market.
- Competitive edge.
Strategic Acquisitions
Elevance Health's strategic acquisitions, like Paragon Healthcare, Inc., are key. They boost care management and fit the goal of comprehensive care. These moves drive growth and diversification, solidifying Elevance Health's leadership. In 2024, Elevance Health's revenue reached $171.3 billion, showing the impact of these strategies.
- Acquisitions enhance care programs.
- They align with Elevance Health's vision.
- These acquisitions support growth.
- Elevance Health aims to be a healthcare leader.
Elevance Health's "Stars" are high-growth, high-share segments. These include ACA exchange plans, commercial fee-based membership, and strategic acquisitions. They drive revenue and market leadership. The company's ACA individual exchange business saw 30%+ growth in 2024.
| Segment | 2024 Performance Highlights | Strategic Implications |
|---|---|---|
| ACA Exchange | 30%+ growth; innovative products. | Market expansion & customer acquisition. |
| Commercial Fee-Based | Revenue increase; strong value. | Enhanced market share & employer value. |
| Strategic Acquisitions | Care program enhancement. | Strategic growth. |
Cash Cows
Elevance Health's BlueCard program offers broad healthcare access. This program is a steady revenue source, boasting a strong market presence. In 2024, BlueCard facilitated a significant volume of healthcare services, contributing substantially to Elevance Health's revenue. Its mature market position indicates stable, predictable cash flow, essential for the company.
Elevance Health's employer group risk-based plans are a core revenue driver. These plans, serving a vast customer base, ensure steady cash flow. They require less investment in rapid expansion. In 2024, this segment contributed significantly to the company's financial stability.
CarelonRx, part of Carelon, boosts Elevance Health's revenue via pharmacy sales. PBM services are a stable market, ensuring consistent demand. In 2024, Elevance Health's revenue reached $171.3 billion, partly from PBM. This makes PBM a reliable cash cow.
Specialty Insurance Products
Elevance Health's specialty insurance, including dental, vision, and disability, is a cash cow. These products cater to stable niche markets, ensuring consistent revenue streams. They require minimal additional investment for growth, making them highly profitable. In 2024, the specialty business segment generated substantial revenue, reflecting its cash cow status.
- Consistent Revenue: Stable demand ensures predictable income.
- Minimal Investment: Low growth investment needs.
- High Profitability: Generates significant cash flow.
- Market Focus: Serves niche markets effectively.
Federal Employee Program (FEP)
The Federal Employee Program (FEP) is a key cash cow for Elevance Health. It offers health benefits to a stable base of federal employees, ensuring consistent revenue. This program typically experiences low growth, but provides reliable financial returns. In 2024, Elevance Health's revenue from government business, which includes FEP, was approximately $25 billion.
- Stable customer base: Federal employees.
- Consistent revenue: Low growth, reliable returns.
- 2024 Revenue: Roughly $25B from government business.
Elevance Health's cash cows generate steady revenue. These include BlueCard and employer plans. In 2024, the PBM segment added to its financial stability.
| Cash Cow | Key Features | 2024 Performance Highlights |
|---|---|---|
| BlueCard | Broad healthcare access | Significant healthcare service volume |
| Employer Group Plans | Core revenue driver | Contributed to financial stability |
| CarelonRx (PBM) | Pharmacy sales | Revenue reached $171.3B |
Dogs
Elevance Health faces Medicaid membership challenges due to eligibility reviews and market exits. Plans in markets with low growth and market share may be "dogs". In 2024, Medicaid attrition impacted revenues. Divestiture or restructuring may be considered for underperforming plans.
Elevance Health has withdrawn from underperforming Medicare Advantage markets, trimming benefits in others. These plans, suffering from low profitability and growth, fit the "dogs" category. In 2024, UnitedHealthcare saw a 7.7% Medicare Advantage growth, showing market shifts. These plans may not offer significant returns.
Elevance Health divested its life and disability businesses to StanCorp Financial Group, Inc. These businesses, marked by low growth, were classified as "dogs" in its BCG matrix. This strategic move, completed in 2024, improved Elevance's focus. The divestiture, a practical choice, streamlined operations.
Smaller, Less Profitable Product Lines
Certain smaller, less profitable product lines within Elevance Health's vast portfolio could be classified as dogs. These segments, struggling with low market share and limited growth potential, demand strategic attention. The company may consider divestiture or restructuring to improve overall profitability. For example, in 2024, Elevance Health's Medicare Advantage plans faced scrutiny.
- Divestiture
- Restructuring
- Low market share
- Limited growth
Plans with Declining Enrollment
Elevance Health might identify some health plans as "dogs" if they face consistent enrollment declines, especially in competitive areas. These plans often struggle to gain or keep members, signaling a need for strategic changes or even considering exiting the market. For example, in 2024, certain regional plans saw a 5% to 10% reduction in enrollment due to aggressive pricing by competitors.
- Market Competition: Intense competition in specific regions can lead to enrollment declines.
- Strategic Intervention: Requires a reassessment of the plan's value proposition or operational adjustments.
- Financial Performance: Plans with declining enrollment usually have lower revenues, affecting overall profitability.
Elevance Health labels underperforming plans as "dogs" in its BCG matrix, focusing on market share and growth. Medicaid and Medicare Advantage plans facing enrollment declines or low profitability are prime examples. In 2024, several regional plans experienced enrollment drops due to intense market competition.
| Category | Characteristics | Actions |
|---|---|---|
| Dogs | Low market share, limited growth, declining enrollment. | Divestiture, restructuring, market exit. |
| Examples | Medicaid plans in competitive areas, underperforming Medicare Advantage plans. | Enrollment declines of 5-10% in 2024. |
| Financial Impact | Lower revenues and overall profitability. | Strategic intervention or operational adjustments. |
Question Marks
Carelon's digital health solutions are a high-growth, low-share segment for Elevance Health. These require substantial investment for market penetration. In 2024, Elevance Health invested heavily in digital platforms, aiming for a larger market share. Success could transform these into high-performing "stars."
Elevance Health's value-based care initiatives strive for better health outcomes and lower costs. These programs, though promising, are still developing and need significant investment for broader reach. In 2024, Elevance Health's revenue reached $171.3 billion, demonstrating its financial capacity to support these initiatives. However, market penetration remains a challenge.
Elevance Health's community health programs, backed by the Elevance Health Foundation, focus on high-growth areas like food security and maternal health. These initiatives, while promising, currently operate within a limited market scope. Expanding these programs requires strategic investments to increase their impact and market penetration. For instance, in 2024, the Foundation invested $50 million in community health programs.
Partnerships with Tech Companies
Elevance Health's tech partnerships aim to boost services but are still gaining ground. These collaborations, vital for future growth, need strategic focus and investment. The goal is to become a market leader. In 2024, Elevance Health invested \$300 million in digital health initiatives.
- Partnerships offer new service opportunities.
- Investments are key for market leadership.
- Strategic alignment is essential for success.
- Elevance Health aims for future growth.
New Market Expansion
Elevance Health's new market expansions are categorized as question marks in the BCG matrix. These initiatives involve substantial upfront investments with uncertain returns. The success hinges on market acceptance and competition, with potential to become stars. If successful, these ventures could significantly boost revenue and market share. For example, in 2024, Elevance Health invested heavily in expanding its telehealth services.
- Requires significant investment.
- Faces uncertainties in market acceptance.
- Competition is a key factor.
- Potential to become a star.
Elevance Health's "Question Marks" involve high investment with uncertain returns, essential for future growth. The success of these initiatives depends on market acceptance and competitive landscape. In 2024, telehealth investments were a key focus, reflecting strategic moves.
| Category | Investment Focus | 2024 Data |
|---|---|---|
| Market Expansion | Telehealth, New Services | $300M in Digital Health |
| Key Challenges | Market Acceptance, Competition | Revenue growth potential |
| Strategic Goal | Transform to "Stars" | Expand Market Share |
BCG Matrix Data Sources
The Elevance Health BCG Matrix utilizes comprehensive financial data, industry analysis, and market reports, offering actionable insights.