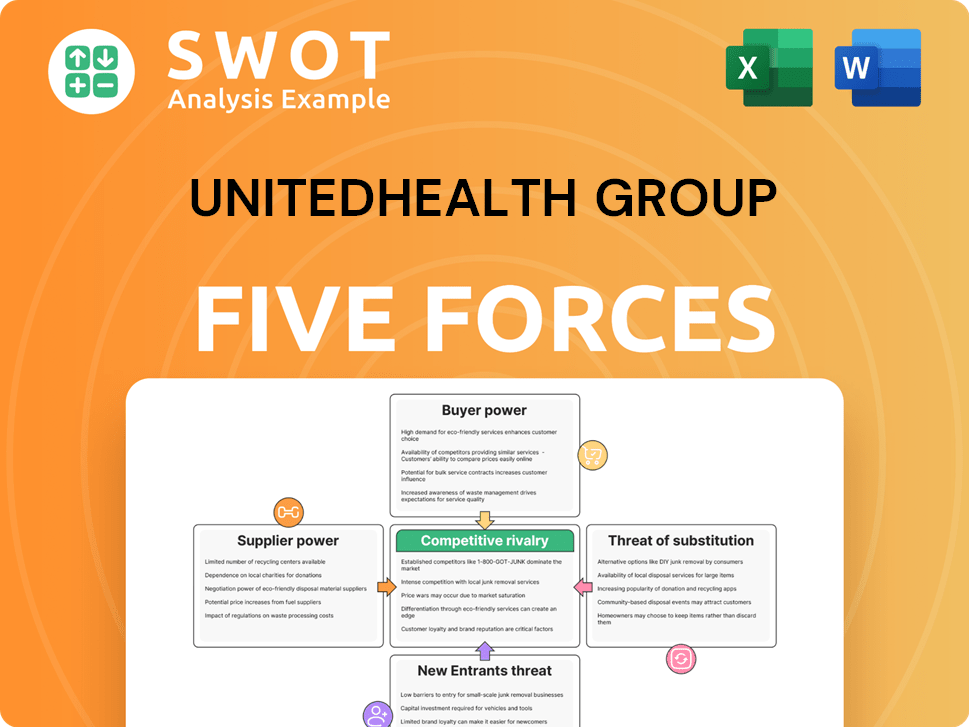
UnitedHealth Group Porter's Five Forces Analysis
Fully Editable
Tailor To Your Needs In Excel Or Sheets
Professional Design
Trusted, Industry-Standard Templates
Pre-Built
For Quick And Efficient Use
No Expertise Is Needed
Easy To Follow
UnitedHealth Group Bundle
What is included in the product
Evaluates control held by suppliers and buyers, and their influence on pricing and profitability.
Quickly assess competitive intensity with a color-coded, easy-to-read layout.
Same Document Delivered
UnitedHealth Group Porter's Five Forces Analysis
This is the complete, ready-to-use analysis file. The UnitedHealth Group Porter's Five Forces analysis examines the competitive landscape, assessing threats from new entrants and substitutes. It also investigates the bargaining power of suppliers and customers. This professionally written document will be ready for your needs. What you're previewing is what you get.
Porter's Five Forces Analysis Template
UnitedHealth Group (UNH) faces a complex healthcare landscape. Buyer power, primarily from large employers & government, significantly impacts pricing. Supplier power, notably from pharmaceutical companies, also presents a challenge. The threat of new entrants is moderate due to high barriers. Intense rivalry exists with competitors like CVS Health. The threat of substitutes, e.g., telehealth, is growing.
Ready to move beyond the basics? Get a full strategic breakdown of UnitedHealth Group’s market position, competitive intensity, and external threats—all in one powerful analysis.
Suppliers Bargaining Power
Consolidation among healthcare providers, like hospitals and physician groups, strengthens their bargaining power. This gives providers leverage to demand higher reimbursement rates from insurers, including UnitedHealth Group. For example, in 2024, mergers and acquisitions in the healthcare sector continued, increasing provider concentration. This trend allows providers to negotiate better terms.
Suppliers of specialized pharmaceuticals wield considerable power, especially when their products lack alternatives. The escalating costs of prescription drugs, particularly specialty medications, pose a challenge to UnitedHealth Group's profitability. In 2024, the pharmaceutical industry saw a 12% increase in specialty drug spending. The Inflation Reduction Act aims to curb these costs, but its complete effect is still unfolding.
Healthcare technology vendors, supplying crucial software and IT, hold significant sway. UnitedHealth Group depends on these vendors for data and operations, creating a dependency. For instance, the global healthcare IT market was valued at $278.3 billion in 2023. Investing in AI and digital health can lessen this reliance.
Healthcare Staffing Agencies
Healthcare staffing agencies wield significant power due to the persistent shortages of nurses and physicians. These shortages drive up labor costs, impacting UnitedHealth Group's expenses, particularly in its Optum Health division. In 2024, the U.S. healthcare sector faced a critical need for professionals, with over 100,000 vacancies for registered nurses. Organized labor's growing influence further strengthens staffing agencies' position.
- Labor costs increased by 5-7% in 2024 due to staffing shortages.
- Optum Health's operating costs rose by 3% in Q3 2024 because of these pressures.
- Unionization efforts in healthcare grew by 10% in 2024.
Third-Party Administrators (TPAs) and Pharmacy Benefit Managers (PBMs)
UnitedHealth Group, despite owning OptumRx, a Pharmacy Benefit Manager (PBM), still deals with other PBMs and Third-Party Administrators (TPAs). These suppliers hold substantial sway over drug prices and formulary choices. The Centers for Medicare & Medicaid Services (CMS) proposed a rule in 2024 to increase transparency in drug pricing, potentially affecting PBMs. This includes requiring PBMs to report rebates and discounts.
Increased regulatory scrutiny and potential reforms aimed at PBM practices could significantly influence UnitedHealth Group's bargaining power. The company's negotiations with these suppliers are pivotal for cost management. In 2023, OptumRx generated $115.6 billion in revenue.
Changes in PBM practices could affect the company's profitability and market dynamics. For instance, the Inflation Reduction Act of 2022 allows Medicare to negotiate drug prices, impacting PBMs. The outcome of these negotiations and regulatory changes is crucial.
- OptumRx generated $115.6 billion in revenue in 2023.
- CMS proposed a rule in 2024 to increase drug pricing transparency.
- The Inflation Reduction Act of 2022 allows Medicare to negotiate drug prices.
UnitedHealth Group faces supplier power challenges from healthcare providers, especially post-mergers, and specialized pharmaceutical companies with essential products. Healthcare IT vendors and staffing agencies, due to shortages, also exert considerable influence. PBMs and TPAs also hold significant sway over drug prices and formulary choices, impacting the company's cost management.
| Supplier Type | Impact on UnitedHealth Group | 2024 Data/Trends |
|---|---|---|
| Healthcare Providers | Demand higher reimbursement rates. | Continued M&A activity increased provider concentration. |
| Specialty Pharmacies | Increased drug costs. | Specialty drug spending rose by 12%. |
| Healthcare IT Vendors | Dependency for data & operations. | Global healthcare IT market valued at $278.3B (2023). |
| Staffing Agencies | Higher labor costs. | Nursing vacancies exceeded 100,000; labor costs increased 5-7%. |
| PBMs/TPAs | Influence drug pricing. | OptumRx generated $115.6B in revenue (2023); CMS proposed drug pricing rules. |
Customers Bargaining Power
Large employer groups significantly influence UnitedHealth Group's profitability. These groups, including entities like the U.S. government and major corporations, negotiate favorable premium rates. UnitedHealth's revenue from these groups was approximately $257 billion in 2024. They have the leverage to demand cost-effective plans. Switching insurers is a real threat, impacting market share.
Government entities, like Medicare and Medicaid, have substantial bargaining power. They influence UnitedHealth Group's finances through reimbursement rates and policy. In 2024, UnitedHealth derived approximately 40% of its revenues from government-sponsored programs. Negative rate pressures and insufficient Medicaid funding remain challenges.
Individual consumers possess a degree of bargaining power, amplified by digital tools and transparency. They can compare health plans and track claims effectively. However, their influence is constrained by network limitations and the intricacy of health insurance. UnitedHealth Group's revenue in 2024 reached approximately $411.5 billion. This influences consumer choices.
Price Sensitivity
Consumers' price sensitivity is growing, particularly due to escalating healthcare expenses. Economic instability can heighten this, pushing individuals to pursue cheaper insurance or forgo it entirely. For instance, in 2024, healthcare spending in the U.S. reached approximately $4.8 trillion. This sensitivity directly influences UnitedHealth Group's capacity to increase premiums.
- Rising healthcare costs make consumers more price-conscious.
- Economic downturns can reduce insurance affordability.
- This affects UnitedHealth Group's premium-setting power.
ACA Marketplace Enrollees
ACA marketplace enrollees have bargaining power, especially with subsidies and enrollment periods. Changes to ACA policies, such as subsidy adjustments, greatly influence enrollment, affecting UnitedHealth Group's market share. Proposed eligibility rules also shift consumer dynamics. These dynamics are crucial for UnitedHealth Group's strategic planning.
- In 2024, approximately 16.3 million people enrolled in ACA marketplace plans.
- The Kaiser Family Foundation reports that the expiration of enhanced subsidies could significantly increase premiums.
- Proposed rule changes could affect the 2025 enrollment period.
Customers' bargaining power significantly impacts UnitedHealth Group's financials. Large groups negotiate favorable rates, as seen in 2024 with $257B revenue from these entities. Price sensitivity due to rising costs and economic factors further influences premium setting.
| Customer Segment | Bargaining Power | 2024 Impact on UnitedHealth |
|---|---|---|
| Large Employers | High | $257B Revenue |
| Government Programs | High | ~40% of Revenue |
| Individual Consumers | Moderate | Influenced by Price |
Rivalry Among Competitors
The healthcare market is fiercely competitive. UnitedHealth Group competes with major insurers like Anthem, Cigna, and Humana. In 2024, the top five US health insurers controlled ~70% of the market. New tech companies are also entering the fray.
Health insurance markets show high concentration, with major players like UnitedHealth Group holding substantial market share. This concentration fuels fierce rivalry as companies vie for members and contracts. The top five insurers controlled over 70% of the commercial market in 2024. The American Medical Association (AMA) actively monitors competition, noting potential anticompetitive effects from consolidation.
Mergers and acquisitions (M&A) significantly shape competitive dynamics in healthcare. UnitedHealth Group's Change Healthcare acquisition, though scrutinized, shows M&A's importance. In 2024, healthcare M&A reached $100B, highlighting its impact. Increased M&A can heighten competition, altering market structures.
Innovation and Technology
Innovation and technology are crucial in the competitive landscape. Companies are heavily investing in digital health platforms, AI, and telehealth. UnitedHealth Group, through Optum, focuses on efficiency, customer engagement, and differentiation. Rapid growth in health tech intensifies competition.
- Optum's revenue grew to $223.3 billion in 2023, a 21.6% increase year-over-year.
- Telehealth adoption increased, with usage rates up by 38% in 2024.
- AI in healthcare is projected to reach $60 billion by 2027.
Cost Control
Managing healthcare expenses is a primary competitive battleground. UnitedHealth Group uses cost-control measures, like pre-authorization, to manage medical costs. Their capability to control costs and offer competitive pricing is crucial for retaining its market position. In 2024, UnitedHealth's medical care ratio was around 83.3%, indicating effective cost management.
- Cost control is vital for competitive advantage.
- UnitedHealth uses pre-authorization and negotiated pricing.
- Competitive pricing is key to market position.
- In 2024, the medical care ratio was approximately 83.3%.
UnitedHealth faces intense competition within the concentrated health insurance market. Key rivals include Anthem, Cigna, and Humana, with the top five insurers controlling roughly 70% of the US market in 2024. Mergers and acquisitions further reshape the competitive landscape, exemplified by UnitedHealth's Change Healthcare acquisition.
Technological advancements, especially in digital health and AI, drive rivalry, as companies invest heavily in innovation. Cost management is also a critical competitive factor; in 2024, UnitedHealth's medical care ratio was about 83.3%.
The competitive environment is dynamic and influenced by several factors.
| Factor | Description | Impact |
|---|---|---|
| Market Concentration | Top 5 insurers control ~70% market share (2024). | High rivalry, price wars, and market share battles. |
| Mergers & Acquisitions | Healthcare M&A reached $100B in 2024. | Changes market structure, increases competition. |
| Technological Innovation | Growing investment in digital health and AI. | Enhances efficiency and customer engagement. |
| Cost Management | UnitedHealth's medical care ratio ~83.3% (2024). | Crucial for competitive pricing and market position. |
SSubstitutes Threaten
Telehealth and virtual care pose a threat, offering alternatives to traditional in-person care. Expanded coverage for online services like mental health reduces reliance on standard plans. UnitedHealth Group integrates telehealth but faces competition from standalone providers. The global telehealth market was valued at $62.2 billion in 2023 and is projected to reach $337.5 billion by 2030.
Direct Primary Care (DPC) models, where patients pay a monthly fee, pose a threat to traditional insurance like UnitedHealth Group. DPC's growth offers a substitute for certain health insurance aspects. In 2024, DPC practices are expanding, attracting patients seeking affordable primary care. UnitedHealth Group must adapt its services to compete with this evolving landscape.
The rise of wellness programs and preventive care poses a threat to traditional healthcare models. These programs, offering services like free screenings and fitness incentives, aim to lower overall healthcare costs by focusing on prevention. UnitedHealth Group is actively incorporating preventive care into its plans to address this shift. For instance, in 2024, UnitedHealth's wellness programs saw a 15% increase in member participation, reflecting a growing trend. This proactive approach helps mitigate the impact of reduced demand for reactive medical services.
Government Healthcare Programs
Government healthcare programs, such as Medicare and Medicaid, represent a significant substitute for UnitedHealth Group's private insurance offerings. The Centers for Medicare & Medicaid Services (CMS) projects that national health spending will reach $7.7 trillion by 2026. Expansions in these government programs, like the potential for increased coverage or added benefits, directly impact the demand for private health insurance products. UnitedHealth Group must strategically navigate these changes to protect its market share and ensure continued profitability in a dynamic healthcare landscape.
- Medicare and Medicaid are major substitutes for private insurance.
- Changes in government healthcare policies can alter demand for private insurance.
- UnitedHealth Group needs to adapt to maintain market position.
- National health spending is projected to increase significantly.
Alternative Medicine and Holistic Treatments
Alternative medicine and holistic treatments are becoming more popular, posing a potential threat to traditional healthcare. These options, while not direct substitutes for health insurance, can decrease demand for specific medical services and medications. UnitedHealth Group must assess how this shift affects its business model. The growing interest in such treatments is a factor to consider in their strategic planning.
- The global alternative medicine market was valued at $82.75 billion in 2023.
- By 2030, the market is projected to reach $157.77 billion.
- Consumer spending on complementary health approaches in the U.S. reached $43.4 billion in 2023.
- UnitedHealth Group's revenue for 2023 was $371.6 billion.
Telehealth, DPC models, and wellness programs challenge traditional care. Government programs and alternative medicine also act as substitutes. These alternatives impact demand and require strategic adaptation from UnitedHealth Group. The company's 2023 revenue was $371.6 billion.
| Substitute | Impact | Data |
|---|---|---|
| Telehealth | Offers virtual care alternatives. | Global telehealth market: $62.2B (2023), $337.5B (2030). |
| Direct Primary Care | Provides direct, affordable primary care. | DPC practices expanding in 2024. |
| Wellness Programs | Focus on prevention, cost reduction. | UnitedHealth's wellness participation up 15% in 2024. |
Entrants Threaten
Entering the health insurance market demands substantial capital. UnitedHealth Group, for example, has a market cap exceeding $450 billion as of late 2024, reflecting the immense resources needed. Constructing provider networks and handling regulatory compliance are costly, creating barriers. This financial burden significantly limits the number of new competitors.
UnitedHealth Group faces significant threats from new entrants due to regulatory hurdles. The healthcare sector is highly regulated at all levels, creating barriers. For example, obtaining licenses and complying with HIPAA can be costly and time-consuming. These regulatory burdens effectively limit the number of new competitors. In 2024, healthcare spending in the U.S. reached approximately $4.8 trillion, highlighting the stakes and regulatory complexity.
UnitedHealth Group's (UNH) established networks of providers, hospitals, and physicians create a significant barrier for new entrants. These relationships, crucial for healthcare delivery, take years to cultivate and maintain, offering UNH a distinct advantage. In 2024, UNH's subsidiary, UnitedHealthcare, managed care for approximately 51.5 million people. Building such a vast network is a resource-intensive process that new companies struggle to replicate quickly. This advantage helps UNH maintain its market position.
Brand Reputation and Trust
UnitedHealth Group's strong brand reputation and customer trust create a significant barrier. New healthcare entrants struggle to match the established trust levels of industry leaders. This trust is critical, as consumers rely on healthcare providers for essential health decisions. For instance, UnitedHealth Group's brand value in 2024 was estimated at $25 billion, highlighting its market strength.
- Brand Recognition: UnitedHealth Group's high brand recognition offers a competitive advantage.
- Customer Loyalty: Established trust fosters customer loyalty, making it hard for newcomers to compete.
- Regulatory Compliance: Maintaining trust helps in navigating the complex regulatory landscape.
- Market Share: A strong reputation supports maintaining and expanding market share.
Economies of Scale
UnitedHealth Group (UNH) thrives on economies of scale, giving it a competitive edge. This allows UNH to offer better pricing and manage operations more efficiently than smaller companies. New entrants often struggle to match these cost structures and operational efficiencies. In 2024, UNH's revenue reached approximately $372 billion, highlighting its substantial scale. This scale presents a major hurdle for new companies trying to compete in the market.
- UNH's 2024 revenue was around $372 billion, demonstrating significant scale.
- Economies of scale lead to lower operational costs.
- New entrants face challenges in achieving similar cost structures.
- Operational efficiency is a key benefit of scale.
New entrants face high barriers. Healthcare requires substantial capital; UnitedHealth's market cap is over $450B. Regulatory hurdles, like HIPAA compliance, are costly. Building provider networks also takes years, limiting competition.
| Barrier | Impact | Example |
|---|---|---|
| Capital Costs | High initial investment | UNH's market cap: ~$450B (2024) |
| Regulation | Compliance is costly & time-consuming | Healthcare spending in U.S. ~$4.8T (2024) |
| Networks | Takes years to build | UNH's managed care: ~51.5M (2024) |
Porter's Five Forces Analysis Data Sources
We utilize SEC filings, financial reports, and industry analyses to construct a comprehensive Porter's Five Forces assessment.